VUR: Managing Backflow for Healthy Kidneys
we work hard to meet your needs
"Protecting Young Kidneys, One Step at a Time."
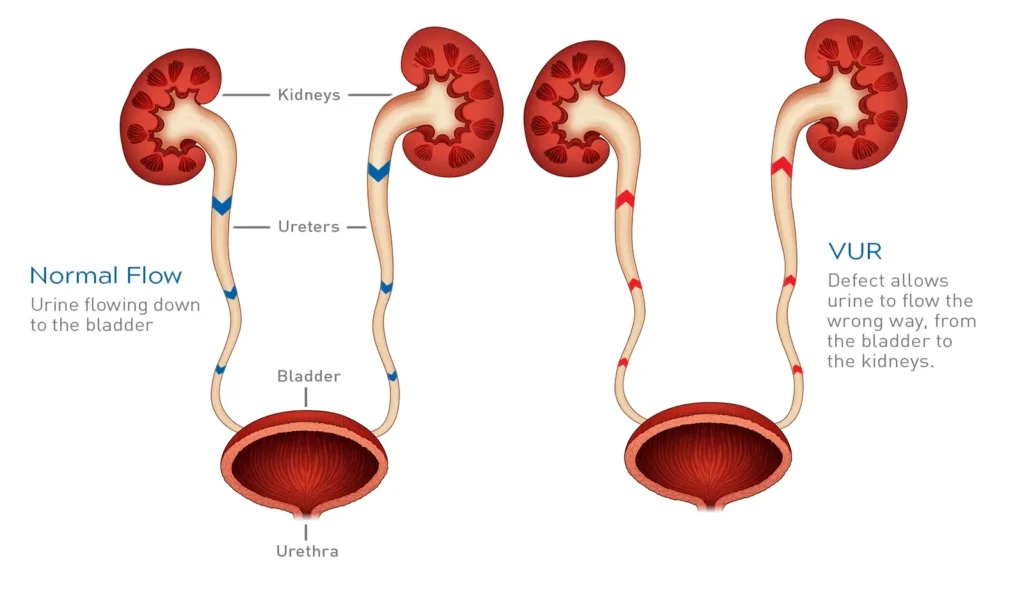
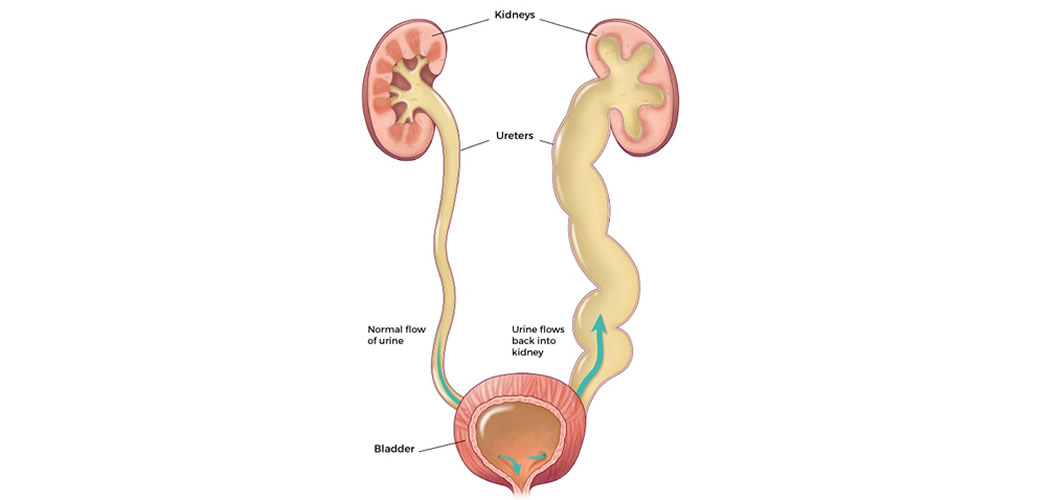
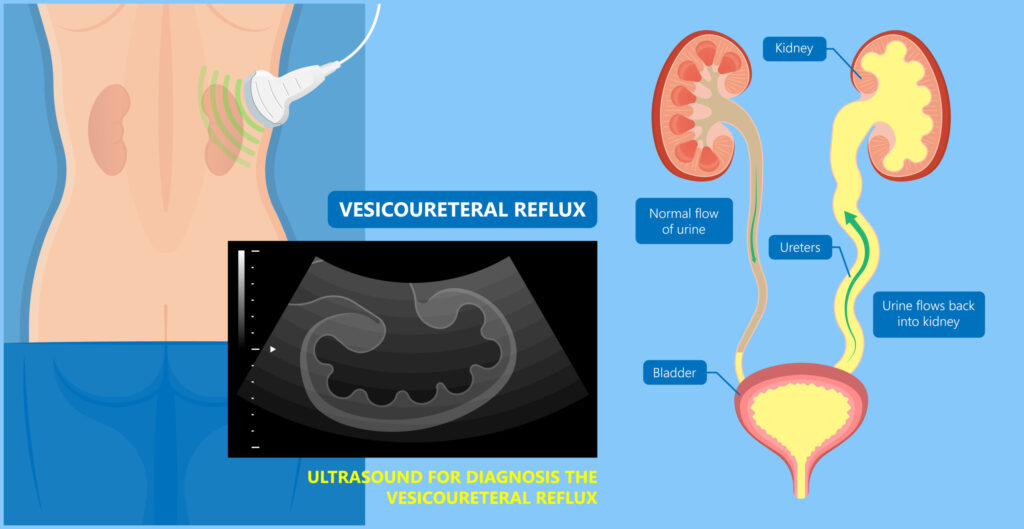
Vesicoureteral reflux (VUR) is a health condition wherein there is a backward flow of urine from the bladder into one or both of the ureters and in some cases back up to the kidneys. Typically, urine flows from the kidneys, through the tubes known as the ureters, into the bladder. The urine is then retained in the bladder until the time of micturition. In VUR, there is a critical reversal that occurs because of a faulty valve which joins the ureter to the bladder.
Types of VUR
Primary (or Essential) VUR
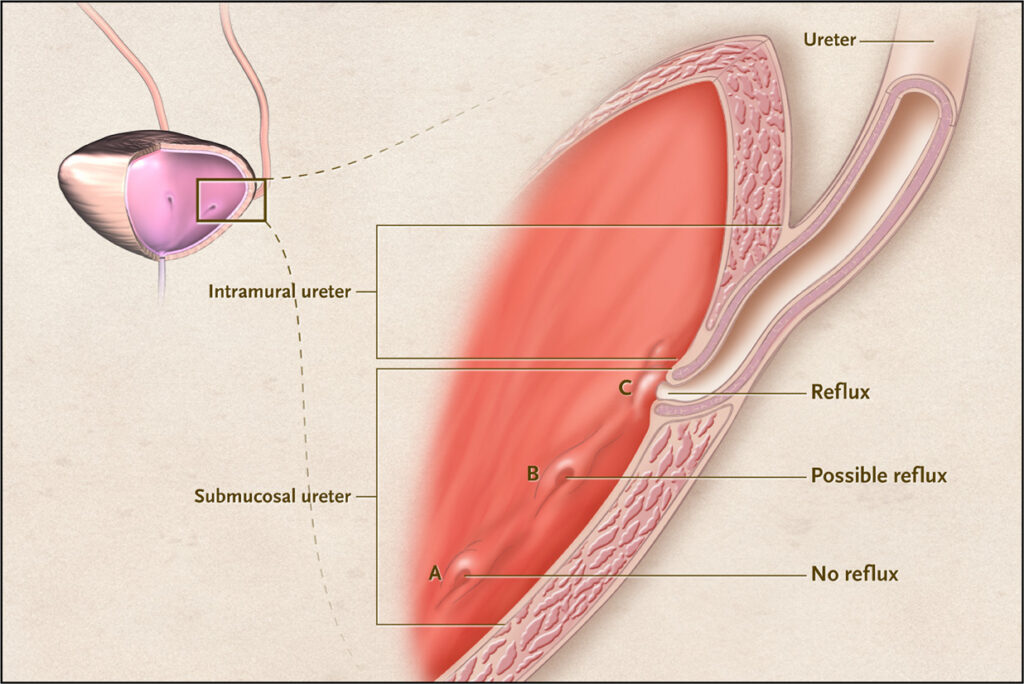
This occurs because of a primary abnormality, which is believed to be due to a genetic defect in the valve, located at the vesicoureteric junction. This is the most common and frequently detected in infants and early childhood.
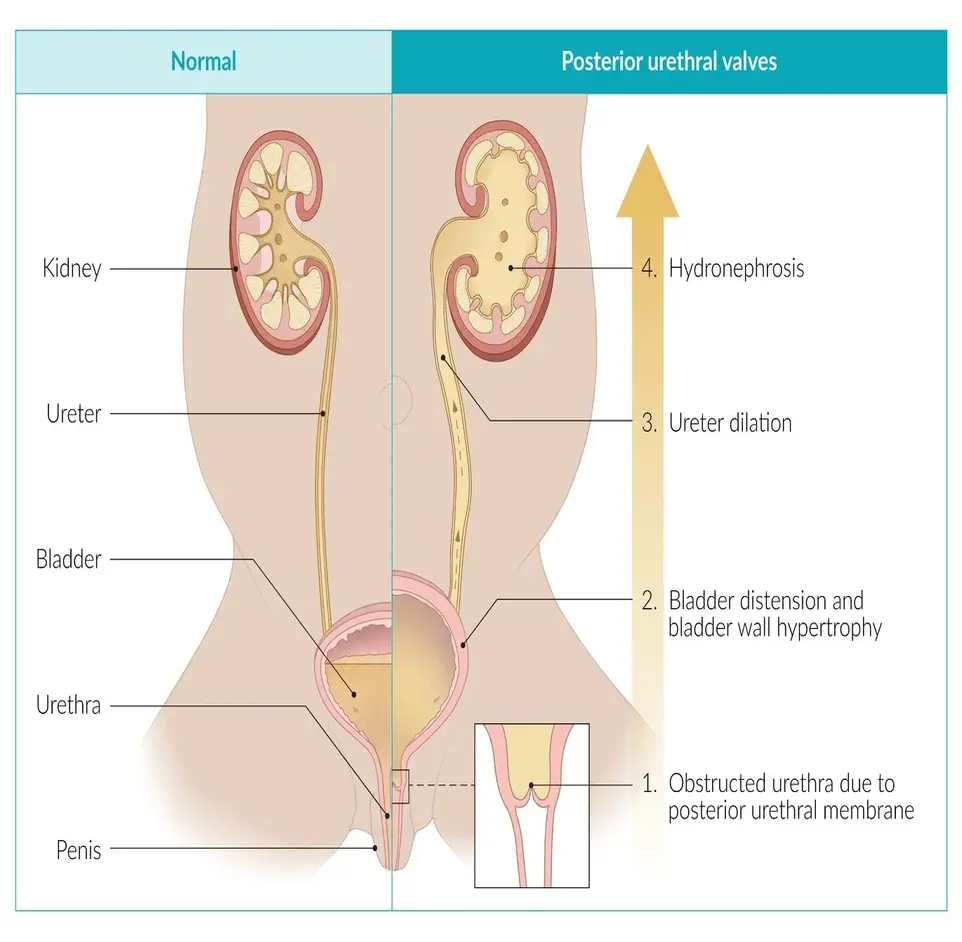
Secondary VUR
It is caused by an obstruction or abnormal pressure, in the bladder, causing backflow. This may occur following urinary tract infections (UTIs) or bladder overactivity.
Symptoms
-
Recurrent urinary tract infections
-
Dysuria
-
Pain in the abdomen or flank region
-
Marked hypertension in terrible forms
-
Chills (when with UTI)
Diagnosis
Voiding cystourethrogram
X-ray demonstrating the picture of the bladder and urethra during voiding and fluid filling of the bladder.
Ultrasound
For evaluating for kidney swelling (hydronephrosis) or other pathological findings.
Functional renal imaging studies
To evaluate renal perfusion and find out about scarring.
Treatment Of Vesicoureteral reflux
Monitoring and Observation
Mild Cases (Grades I and II): In cases of mild VUR, particularly in young patients, the condition may improve naturally within a certain period as the patient grows. There is often advice on longitudinal follow-up, including imaging for VUR.
Preventive Care: Parents should be instructed about the signs and symptoms of a UTI and should alert the child’s physician if such symptoms occur.
Antibiotic Prophylaxis
Low-Dose Antibiotics: Low-dose prophylactic antibiotics are indicated for children with VUR who are prone to UTI recurrence or those with high-grade reflux, to be taken every day. This will prevent any further infections that can cause damage to the kidneys.
Regular Urine Tests: On the other hand, during treatment with antibiotics, regular urine tests may be conducted to deter infections.
Types of Surgery
Ureteral Reimplantation: This is the most frequent intervention employed in VUR patients where ureters are re-placed in their position with a better-designed valve and thus are prevented from regressing.
Endoscopic Injection: A procedure which is less invasive in which a material is injected into the vicinity of the ureter to help prevent the opening as a result of reflux. This kind of approach is often reserved for moderate Ones of VUR.
Behavioural and Lifestyle Alterations
Bladder Training: In some situations specifically for older children bladder training and other bladder management techniques may be warranted to reduce symptoms.
Hydration: Making sure the child drinks a large volume of liquids may assist in washing the bacteria out of the urinary tract thus decreasing the chances of infections occurring.
Regular Follow Up
Imaging Tests: In most patients, repeat imaging studies such as renal ultrasounds or voiding cystourethrograms (VCUG) are routinely done for years to follow the course of the disease.
Kidney Function Tests: Outpatient healthcare providers may order regular kidney function tests to determine any effects of VUR on the child’s kidneys.
Prognosis
Following the right intervention, most of the children suffering from VUR do not develop any long-term kidney injury and go on to live the healthiest of includes. Self-limiting mild ones are better off as they and tough ones can be remedied by surgical or other management approaches.
The choice of treatment is individualized, taking into account the specific needs and health of the patient. Healthcare workers cooperate with the parents of children to achieve the best result possible.
